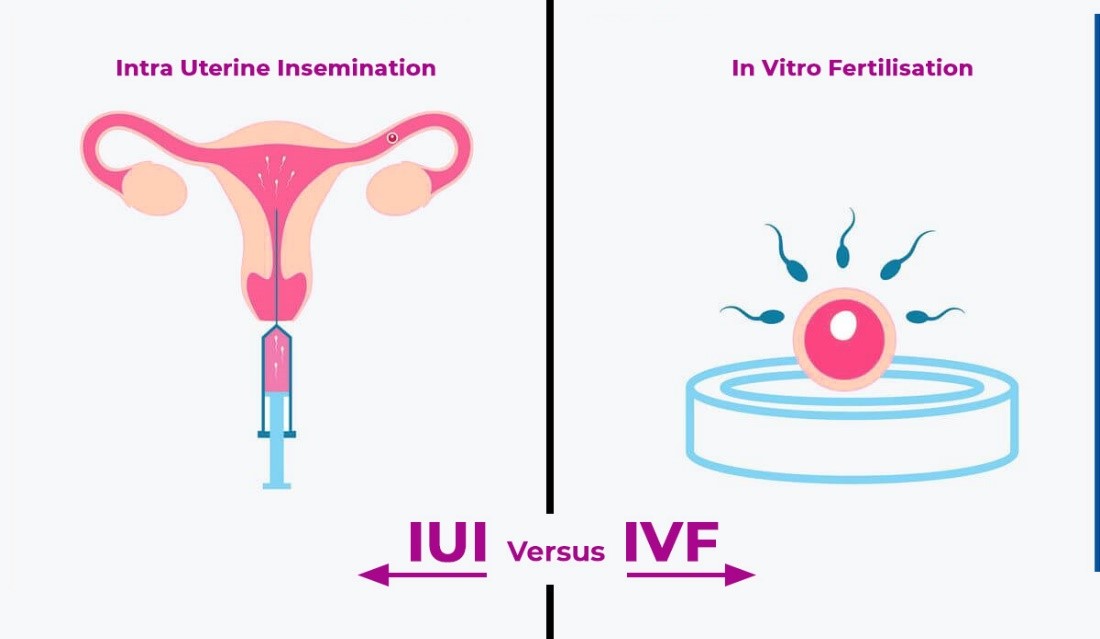
When faced with fertility challenges, many couples and individuals explore assisted reproductive technologies (ART) to help them conceive. Two of the most common options are In Vitro Fertilization (IVF) and Intrauterine Insemination (IUI). Both treatments have helped millions of people start families, but choosing between IVF and IUI can be overwhelming. Understanding the differences between these treatments, how they work, and their success rates is crucial for making the best decision based on individual circumstances.
What is IVF?
In Vitro Fertilization (IVF) is one of the most well-known and advanced forms of fertility treatment. It involves retrieving mature eggs from a woman’s ovaries and fertilizing them with sperm in a laboratory to create embryos. These embryos are then cultured for a few days, and one or more healthy embryos are transferred into the woman’s uterus, where they can implant and develop into a pregnancy.
The IVF process involves several steps:
- Ovarian stimulation: Medications are used to stimulate the ovaries to produce multiple eggs.
- Egg retrieval: A minor procedure is performed to collect the eggs from the ovaries.
- Fertilization: Eggs are fertilized with sperm in a laboratory (through conventional IVF or with ICSI if sperm quality is an issue).
- Embryo culture: The fertilized eggs (now embryos) are monitored for several days.
- Embryo transfer: One or more embryos are transferred to the uterus for implantation.
What is IUI?
Intrauterine Insemination (IUI) is a less invasive fertility treatment compared to IVF. In IUI, sperm is collected, washed, and then directly inserted into the uterus during ovulation to increase the chances of fertilization. The procedure is relatively simple and is often combined with medications to stimulate ovulation.
The IUI process involves:
- Ovulation induction (optional): Medications may be used to stimulate ovulation and increase the number of eggs available.
- Sperm collection and preparation: Sperm is collected from the partner or a donor and washed in a lab to select the healthiest sperm.
- Insemination: The washed sperm is injected directly into the uterus using a catheter.
Success Rates of IVF vs. IUI
The success rates of both treatments vary depending on factors like the patient’s age, cause of infertility, and overall health.
IVF Success Rates
IVF generally has higher success rates compared to IUI, especially for certain infertility factors. According to data from fertility clinics worldwide, the success rates for IVF range between:
- 40-50% per cycle for women under 35.
- 30-40% per cycle for women aged 35-37.
- 20-30% per cycle for women aged 38-40.
- 10-15% per cycle for women over 40.
IVF is often recommended for patients with more complex fertility issues, such as blocked fallopian tubes, severe male factor infertility, or diminished ovarian reserve. It also offers the option of Preimplantation Genetic Testing (PGT), which can screen embryos for genetic abnormalities before transfer, increasing the chances of a successful pregnancy.
IUI Success Rates
IUI has lower success rates compared to IVF, but it is a less invasive and more affordable option. The success rates for IUI are generally:
- 15-20% per cycle for women under 35.
- 10-15% per cycle for women aged 35-40.
- 5-10% per cycle for women over 40.
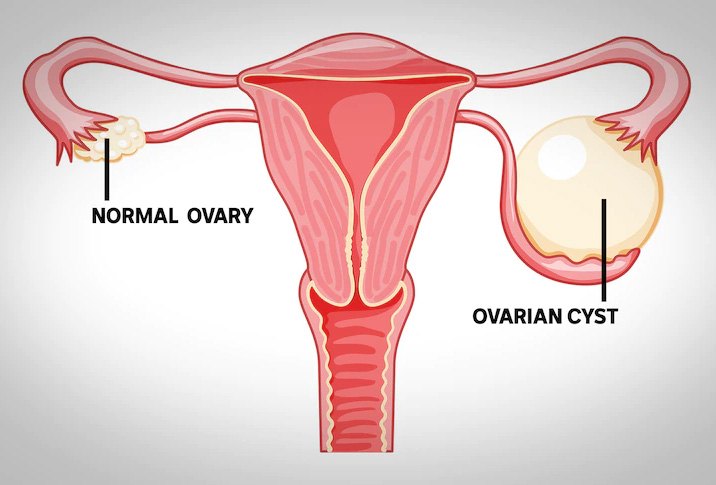
IUI is most effective when the couple’s infertility is unexplained or due to mild male factor infertility. It can also be an option for couples where the woman has regular ovulation, healthy fallopian tubes, and no severe underlying fertility issues. For some, IUI may be the first step before moving on to IVF if it is not successful after several attempts.
Factors to Consider When Choosing IVF or IUI
When deciding between IVF and IUI, several factors should be considered, including:
1. Cause of Infertility
- IVF is often recommended for more severe fertility challenges, such as blocked fallopian tubes, severe male factor infertility, or advanced maternal age.
- IUI is typically used for less complicated cases, such as unexplained infertility, mild male factor infertility, or when the woman’s fallopian tubes are open.
2. Age
- Age plays a significant role in fertility treatment success. Women over 35 are generally more likely to benefit from IVF because the success rates decline more rapidly for IUI in this age group.
3. Cost
- IUI is significantly more affordable than IVF, with a single IUI cycle costing a fraction of an IVF cycle. Many couples opt to try IUI first because it is less invasive and less expensive.
- IVF is more expensive, but its higher success rates, especially for older women or those with more complex fertility issues, often justify the investment.
4. Time
- For couples who have been trying to conceive for a long time or women who are older and concerned about declining egg quality, IVF may offer a faster path to pregnancy.
- IUI is often tried first, especially if the couple is younger or has no severe fertility issues. It’s less invasive, and multiple cycles can be attempted before moving on to IVF.
When is IVF Better?
IVF is generally the better option for patients when:
- There are more complex fertility issues, such as blocked fallopian tubes, severe endometriosis, or poor egg/sperm quality.
- The woman is over 35 and has concerns about egg quality.
- There is a need for genetic testing of embryos to avoid genetic diseases.
- IUI has failed after several attempts.
When is IUI Better?
IUI is a good first-line treatment when:
- The couple is younger (under 35) with mild infertility issues.
- There are no severe male factor fertility issues.
- The woman has healthy fallopian tubes and regular ovulation.
- The couple prefers a less invasive and more affordable option to begin with.
Conclusion: Which is Better for You?
The decision between IVF and IUI depends on the individual or couple’s unique circumstances. IVF is often recommended for those with more complex fertility issues or for women over 35 who are concerned about time and egg quality. On the other hand, IUI may be a good first step for younger patients with milder infertility problems or for those looking for a less invasive and more affordable option.
Ultimately, the best approach is to consult with a fertility specialist who can evaluate your specific fertility challenges and guide you toward the treatment that offers the highest chances of success.
For any of your fertility problems, please do not hesitate to contact us. At Fertility Solutions we pride ourselves with the excellent tailored personal care we provide to our patients for their specific needs. A team member will contact you as soon as we get your message, and construct a personal treatment plan for your fertility problems in the country of Cyprus. You can also contact our clinics directly through the links below.
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi