Sperm Washing: A Crucial Step in Assisted Reproduction
Sperm washing is a vital procedure in assisted reproductive technologies (ART) such as intrauterine insemination (IUI) and in vitro fertilization (IVF). This laboratory process prepares sperm by separating motile, healthy sperm from seminal fluid, dead sperm, and debris, improving the chances of successful fertilization.
What is Sperm Washing?
Sperm washing is a laboratory technique used to enhance the quality of sperm used in fertility treatments. The procedure removes unwanted substances from the semen, including:
- Non-motile and abnormal sperm
- White blood cells and bacteria
- Seminal plasma, which contains prostaglandins that can cause uterine contractions and discomfort
The end result is a concentrated sample of high-quality sperm, which increases the likelihood of fertilization.
Why is Sperm Washing Necessary?
Sperm washing is an essential step in fertility treatments for several reasons:
- Enhancing Fertility Treatments: Sperm washing increases the motility and viability of sperm used in IUI and IVF procedures.
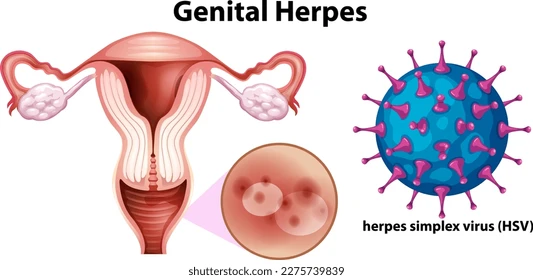
- Preventing Infection: In cases where a male partner has an infection or carries a virus such as HIV or hepatitis, sperm washing helps remove viral particles, reducing the risk of transmission.
- Overcoming Male Factor Infertility: If a man has a low sperm count (oligospermia), poor motility (asthenospermia), or abnormal morphology (teratospermia), washing helps isolate the best sperm for fertilization.
- Removing Antibodies: In cases where antisperm antibodies are present, sperm washing reduces their impact, improving the chances of conception.
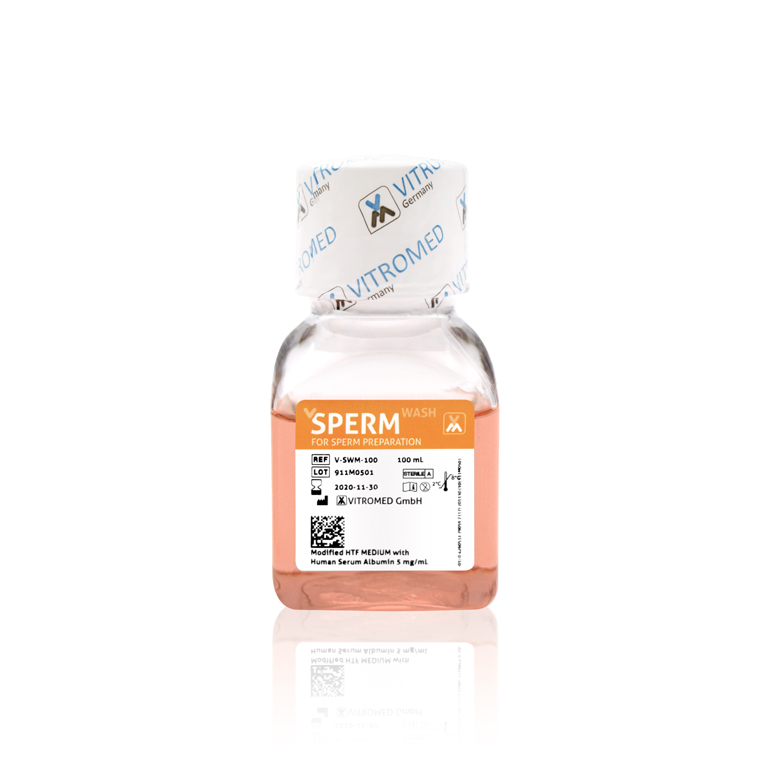
Methods of Sperm Washing
There are different sperm washing techniques, each with its own benefits:
1. Simple Wash Method
- The semen sample is mixed with a washing medium and then centrifuged to separate sperm from seminal fluid.
- The supernatant (fluid containing unwanted cells and debris) is discarded, leaving behind the motile sperm pellet.
- This method is commonly used for IUI but may not be as effective for severe male infertility cases.
2. Density Gradient Centrifugation
- The semen is layered over a density gradient medium and centrifuged.
- High-quality sperm swim through the layers, while dead or immotile sperm and debris remain in the upper layers.
- This method is highly effective for isolating the most motile and morphologically normal sperm, making it ideal for IVF and intracytoplasmic sperm injection (ICSI).
3. Swim-Up Technique
- The semen sample is placed in a culture medium, allowing motile sperm to swim upward while debris and non-motile sperm settle at the bottom.
- The upper layer containing high-quality sperm is then collected.
- This technique is useful when a high concentration of motile sperm is needed.
Sperm Washing and HIV-Positive Patients
For couples where the male partner is HIV-positive, sperm washing is crucial. Research has shown that properly washed sperm samples can significantly reduce the risk of HIV transmission. Many fertility clinics offer this service to help HIV-positive men safely conceive with their partners.
Cyprus Crown IVF and Cyprus American IVF accept male patients, but only those with sexually transmitted diseases (STDs) such as HIV, and they conduct the sperm washing technique to ensure safe fertility treatment.
Success Rates and Considerations
The success of sperm washing depends on several factors, including the quality of the sperm before processing, the method used, and the type of fertility treatment. Clinics with advanced laboratory techniques, such as Cyprus Crown IVF and Cyprus American IVF, ensure optimal sperm preparation for IUI, IVF, or ICSI procedures, increasing the chances of pregnancy.
Conclusion
Sperm washing is an essential process in ART, helping to improve fertilization rates and reduce health risks. By selecting the healthiest and most motile sperm, this technique maximizes the chances of conception for couples facing infertility challenges. Clinics specializing in sperm preparation, such as those in North Cyprus, offer cutting-edge solutions to support individuals and couples on their fertility journey.
For any of your fertility problems, please do not hesitate to contact us. At Fertility Solutions we pride ourselves with the excellent tailored personal care we provide to our patients for their specific needs. A team member will contact you as soon as we get your message, and construct a personal treatment plan for your fertility problems in the country of Cyprus. You can also contact our clinics directly through the links below.
Cyprus Crown IVF Contact: https://en.cypruscrownivf.com/contact
Cyprus American IVF Contact: https://www.cyprusamericanivf.com/contact-us/
Dr. Halil Ibrahim Tekin (Dr. HIT) Youtube: https://www.youtube.com/@dr.halilibrahimtekin1715
Cyprus American IVF Youtube: https://www.youtube.com/@AmerikanTupBebekMerkezi